The fact that “the United States spends more on health care than any other nation in the world, yet it ranks poorly on nearly every measure of health status,” was brought to the spotlight in 2007 by Steven Schroeder, M.D. His impactful talk, “We Can Do Better – Improving the Health of the American People” was a call for change. Yet, a decade later, despite the work of many, this reality stands firm.
Working as a vendor to government social services agencies, GovWebworks has seen the struggles that clients and supporting nonprofits undergo to make a difference in this area.
One of the more promising efforts towards change is the focus on social determinants of health (SDH), the lifestyle factors that have immediate impact on the health of individuals, as discussed in a recent post on the topic. Studies show (Figure 1) that as a determinant of overall health, medical care influences only around 10 percent of the outcome, while other factors such as behavior come in at nearly 40 percent, and socioeconomic status at 20 percent.
The valuable work around improving SDH for citizens is part of an encouraging trend toward prevention. Such action is far preferable to costly, and last-minute, emergency room treatment. However, the best path forward for agencies and organizations looking to offer help is not always clear.
The power of a ZIP code
“The importance of social determinants in population health,” by Harm Scherpbier, MD, and Caitlin Breanne Smith, MPH, of Phillips Wellcentive highlights the studies of David Nash, MD, MBA, dean of Jefferson College of Population Health, and a leading voice on SDH.
“The most important five-digit number I need to predict your health status and wellbeing is your ZIP code, bar none,” Nash says. “It’s not your cholesterol level or your blood pressure number or your age. The No. 1 health predictor is your ZIP code.” (More on this topic in a video from Health Happens Here.)
The example given by Nash is a 2014 study of babies born in Montgomery County, MD. They have a life expectancy six to seven years longer than those born one ZIP code away in Washington, D.C.
“Additionally, we know that patients’ health literacy, education level, geography, and socioeconomic status can have an adverse impact on their access to proper preventive healthcare,” Nash says. “They ultimately cost the healthcare system more because they enter the system when their illness is more severe – usually via the emergency room, the most expensive point of care.”
Nash believes that such groups of patients are the key to a population health approach. This means determining the ZIP code areas where at-risk populations have a lower quality of social determinants of health. Then preventative services can be encouraged for these populations before they get to the point of the emergency room.
It sounds like such a common sense solution, but the variables are many and hard to track. This is where data aggregation can be helpful.
How data can help
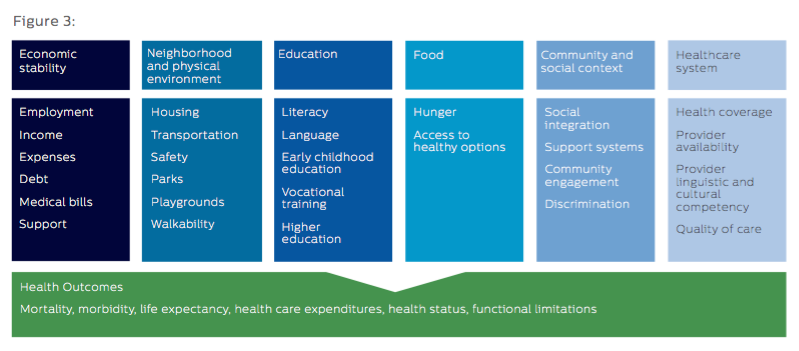
Data collected by Phillips Wellcentive around social determinants of health focuses on six principal socioeconomic factors. These have been identified by the Centers for Disease Control and Prevention (CDC) as primarily responsible for health inequities. They are:
- Economic stability
- Neighborhood and physical environment
- Education
- Food
- Community and social context
- Healthcare systems
The following chart provided by the Kaiser Family Foundation shows how each area encompasses a variety of contributing factors:
Companies such as Phillips Wellcentive aggregate the data around these factors and other issues for individual patients in target groups. This helps to estimate the successful actions medical providers can take to improve clinical and financial results for that group.
Such population health management programs depend on the success of addressing societal needs of patients. This is especially important around housing and food insecurity issues. Studies (Seligman, HealthAffairs) show that “diabetics are 27 percent more likely to be hospitalized in the last week of the month compared to the first week due to exhaustion of food budgets at month’s end.”
As a result, there are many agencies and community based organizations that strive to help struggling communities improve health outcomes. However, it can be difficult to connect the dots between patients and the right social services for their needs. This is where collaboration is necessary.
A collaborative solution
Products such as our CiviServ application and Healthify utilize a database to provide citizens with the most current and geographically relevant services. They also identify the social services that are eligible and available to a given person based on their particular needs.
We think such tools can help agencies and organizations work together to share the financial burden of improving SDH. The rewards of such collaboration can lead to decreased medical costs, and better outcomes for citizens.
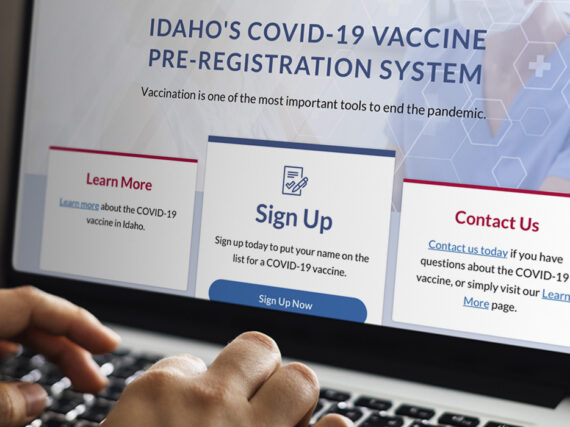
Our clients in the State of Idaho are employing this strategy with the Live Better Idaho database and means testing tool. As detailed in our last post, through self assessment, Idaho citizens can find help based on their specific financial and social circumstances. They can also save information for future reference, and get alerts when new services become available.
Most importantly, the online tool allows the various service providers in the database to work together, and provides a platform for smaller interests that may not otherwise have the funding. This helps get the correct services to the right people. As a result, goals targeting certain populations and ZIP code areas for specific services can more easily be met.
We believe the democratic nature of these tools is the key to improving social determinants of health. It’s our hope that such tools can help to improve the nation’s overall health record, as well.
Driving adoption
Despite the obvious benefits of this approach, many states and counties struggle to pull in the same direction to address social determinants. Often different constituent organizations are competing for funding and attention. Stay tuned for the next post on ways individual interests can work together to improve outcomes.
Learn more
- Targeting Social Determinants of Health: Why Idaho’s online service discovery tool can improve health
- From Single Cause to Macro Solution: How online innovation can bring the right services to more people
- Social Determinants, Illustrated: Infographics explain factors influencing health, and how to address them
- Let us know if you’d like to hear about how we can help align your efforts