The Challenge
While great strides have been made in making it possible for people to apply for benefits online, many still apply in person and on paper, and equal thought needs to be given to that user experience. As the state of Vermont began its journey towards a holistic integrated eligibility application process, one of the first steps it took was in consolidating its many different health and assistance application forms. GovWebworks was selected to assist in this process, based in no small part on our experience in working on integrated eligibility challenges with other states.
Our Approach
Working with Vermont’s Department of Health Access (VDHA), our team began with days of onsite discovery to understand the purpose of each of the forms, who uses them, how and where they are completed, and how they are processed internally. The forms supported the ability to apply for health and pharmacy plans, as well as long-term care and financial assistance in paying for healthcare.
As work progressed, we worked in collaboration with the Department to consolidate common elements, and develop a user-flow that would serve both applicants and internal users. In addition to usability improvements, our team also looked to address readability and comprehension through a focus on the use of plain language. At every step our recommendations were reviewed by subject matter experts at the Department for compliance with the state and federal requirements associated with the programs offered.
Ultimately the integrated eligibility application was refined and validated through three separate rounds of in-person testing, with both applicants and internal staff, to ensure usability throughout completion and processing.

The Results
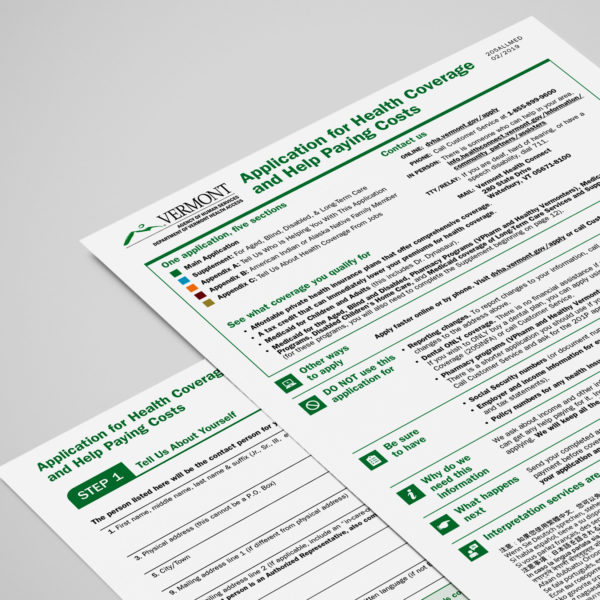
Completed in February 2019, our consolidated forms allowed applicants to self-select health benefits program(s) or request a full health care screening for both Modified Adjusted Gross Income (MAGI) and non-MAGI based eligibility determinations. The application adheres to the Center for Medicaid Services’ Guidance on State Alternative Applications for Health, while using plain language, usability and readability techniques to streamline the completion process.
Ultimately the new, user-centered forms greatly simplifies the application process for Vermonters, while reducing data entry and processing time for VDHA staff. This work is one of the first critical steps for the Department as it looks to integrate its entire benefits application process, both online and offline.


